RSV GOLD III – ICU Network Study
The burden of RSV mortality is highest in low- and lower-middle-income countries (LMICs). However, there is a lack of individual patient data which are essential to inform policy makers about possible target populations for future RSV interventions. Furthermore, awareness on RSV-related disease burden is limited due to lack of diagnostic capacity. We aim to target both problems to pave the way for future vaccine introduction.
The ICU Network Study is an international, prospective, observational multi-centre study conducted in 10 LMICs. We aim to describe clinical, demographic and socioeconomic characteristics of RSV-positive children under 2 years of age who have been admitted with severe RSV infection to the pediatric intensive care unit (PICU) or high dependency unit (HDU).
The study protocol has been published and is accessible here.
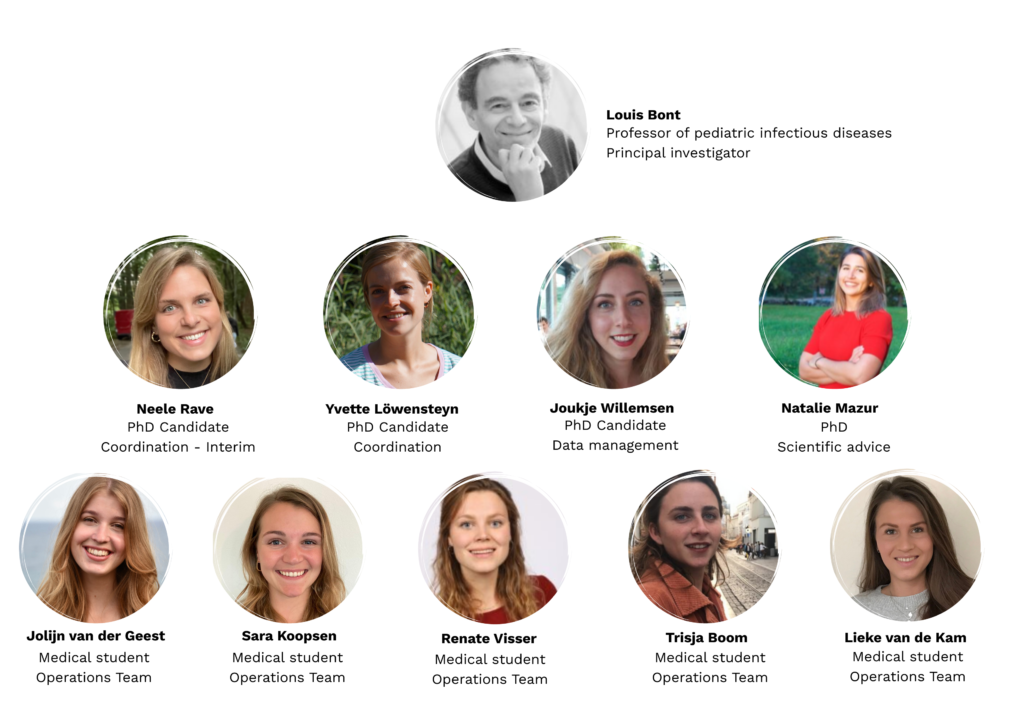
The Dutch organisational study team consists of:
After a careful selection process, we have selected 10 enthusiastic study teams who will perform point-of-care RSV testing during the respiratory season for a duration of 2 years. Our 10 study sites are based in Bolivia, Cameroon, the Gambia, Ghana, Haiti, Mozambique, Nepal, Nigeria, Sudan and Tanzania:
Bolivia
Hospital de Niños “Dr. Mario Ortiz Suarez”, Santa Cruz, Bolivia
Hospital de Niños “Dr. Mario Ortiz Suarez” is a tertiary children’s hospital located in Santa Cruz, the largest city of Bolivia. The 130-bed hospital admits children up until the age of 13 years. Inclusions for the RSV GOLD study will take place at both the PICU and the “Sala de Reanimación”, which serves as an HDU. The PICU has 7 beds and the HDU has 6 beds. Invasive ventilation is available for all beds at both units. Annually, approximately 250 children are admitted to the PICU, of which more than 40% is younger than 2 years. Respiratory season runs from March to October.

Cameroon
Laquintinie Hospital, Douala, Cameroon
The Laquintinie Hospital in Douala is located in the heart of the Akwa district, Douala, Cameroon. It covers 09 hectares, it is a 2nd category referral hospital with a mission to ensure daily quality healthcare management of patients and adapted response towards major events like disasters, epidemics, sporting events, etc. Each year approximately 660 children are admitted to the PICU of which 180 have acute respiratory infections. Most of these respiratory infections occur between the months of April to June and September to January.

The Gambia
Edward Francis Small Teaching Hospital, Banjul, The Gambia
Edward Francis Small Teaching Hospital (EFSTH) is a 540-beds tertiary care facility located in the capital of The Gambia.
The pediatric ward consists of 20 beds and a 12-bed high-dependency unit. The pediatric ICU is a shared ICU for children and adults, consisting of 8 beds, of which up to 6 beds can be used for pediatric admissions. Approximately 100-200 children are admitted with respiratory symptoms each year and approximately 60% are younger than 2 years of age.

Ghana
Korle Bu Teaching Hospital, Accra, Ghana
Korle Bu Teaching Hospital, the premier tertiary healthcare facility in Ghana, was established in 1923. Currently, the hospital, which is the third biggest referral centre in Africa, has 2,000 beds, 21 clinical and diagnostic departments and three Centres of Excellence. It also has an average daily outpatient attendance of 1,500 with about 250 inpatient admissions. It is a teaching hospital affiliated with the University of Ghana Medical School. The Child Health Department of the hospital sees a variety of cases as referrals. The Pediatric ICU is a newly built facility which started operation in November 2019. It has 6 ICU beds with ventilators and 18 high dependency unit (HDU) beds.
Noguchi Memorial Institute for Medical Research (NMIMR), Accra, Ghana
Noguchi Memorial Institute for Medical Research (NMIMR) is a leading medical research institute located at the University of Ghana in Accra, Ghana. It was founded in 1979 with a mandate to improve the health and wellbeing of Ghanaians and mankind through focused and relevant quality biomedical research, human resource developments, specialized diagnostics and support of national public health activities. The NMIMR houses many WHO-accredited laboratories including the National Reference Laboratory for Influenza and Other Respiratory Viruses. Currently, test samples for the COVID-19 pandemic in Ghana are performed and confirmed by the institute.

Dr. Kwabena Osman (consultant pediatrician)

Haiti
Hôpital Saint- Damien / Nos Petits Frères et Sœurs, Port-au-Prince, Haiti
Created and funded by Nuestros Pequenos Hermanos International (NPHI), Saint-Damien is a 188 beds capacity’s Hospital, providing high-quality care to disadvantaged and sick children in Haiti for almost 32 years. The hospital also ensures since 2010 qualified treatment to pregnant women with high risk during their delivery.
Saint – Damien and associated NPH public health programs reach over 80000 children annually in the country. While caring a significant percentage of children with infectious diseases (respiratory infections, HIV, Tuberculosis, Sepsis …), the hospital also offers specialized care through its cancer, cardiac, epileptic, renal, and sickle cell disease units. Saint-Damien staff believed in continuous education. For that reason, with the support of both national and international institutions, the hospital hosted a pediatric residency program and a fellowship in pediatric surgery. Finally HSD is currently expanding its research experience through the Monitoring Evaluation and Research Department, involving clinical and epidemiological projects.

Mozambique

Hospital Central de Maputo, Maputo, Mozambique
The Unidade de Cuidados Intensivos Pediátricos (UCIP) at Hospital Central de Maputo (HCM) is a 24-hour service, integrated into the Paediatric Department at Maputo Central Hospital, the larger and National Reference Hospital in Mozambique.
The unit has currently 18 beds and provides differentiated multidisciplinary medical and surgical care to admitted children from 0 to 14 years in critical condition requiring either medical, surgical, and trauma care, and to those with acute or chronic acute kidney failure requiring renal treatment.
The medical team consists of different professionals who provide personalized care and maximum comfort. This team includes general paediatricians, paediatricians with a subspecialty in paediatric intensive care, nurses, assistants, maids, students, and others. An average PICU day shift has two pediatricians/intensivists, two pediatric residents, four-five nurses and three medical students. The evening shift has one-two pediatricians/intensivists, two pediatric residents, three nurses and two medical students. During the night shift, one pediatrician/intensivist, one pediatric resident, three nurses and two medical students are present.
The UCIP-HCM is also a training unit for medical students and residents and hosts clinical studies and trials, which contributes to training in research. The unit ambitions includes (a) increasing the number of full time local specialized and dedicated staff; (b) improve the capacity of necessary means of monitoring, diagnosis, therapy and research; (c) improve the assistance to burn patients in the Burn Unit (a specialized unit, integrated in the Plastic Surgery Service); (d) create an intermediate care unit to monitor non-invasive or minimally invasive procedures in patients at risk of developing organ dysfunction/failure, and with the capacity to ensure resuscitation manoeuvres in coordination with the PICU.
More information can be found at http://www.hcm.gov.mz



Faculdade de Medicina (FAMED), Universidade Eduardo Mondlane (UEM), Maputo, Mozambique|
FAMED-UEM is the principal medical school in Mozambique, founded in 1962. In addition to the MD program, there are four Masters and one PhD program. FAMED-UEM has a Scientific Council, Institutional Ethical Review Board, 6 Laboratories, 3 research support unit and 2 extension units. It is located at the same campus as HCM.
More information can be found at https://www.med.uem.mz

Nepal
Kanti Children’s Hospital and Tribhuvan University Teaching Hospital, Kathmandu, Nepal
Kanti Children’s Hospital (left on the photo) and Tribhuvan University Teaching Hospital (right on the photo) are public referral hospitals located in Kathmandu, the capital of Nepal. Kanti Children’s Hospital is the only children’s hospital in the country and provides care for children up to 14 years of age. Tribhuvan University Teaching Hospital, located across the street, is a multidisciplinary hospital at the oldest medical school in the country and is a national referral center. The pediatric ward admits patients up to 16 years of age. Each of the hospitals has a dedicated PICU managed by pediatricians and is usually occupied. PICUs in both hospitals have access to basic hematology and electrolyte panels, urinalysis, cerebrospinal fluid studies, blood gas and radiography with portable chest X-ray and a CT scan if required. The respiratory season runs from July until March, with a peak between September – November.

Nigeria
Ahmadu Bello University Teaching hospital (ABUTH), Zaria, Nigeria
ABUTH is a tertiary healthcare facility located in Zaria. It is one of the largest teaching hospitals in Nigeria. The emergency paediatric unit serves as a high dependency unit (HDU) and consists of 32 beds. The NICU has 8 beds. Each year, approximately 140 children are admitted to the HDU with acute respiratory infections, of which 70% are under the age of 2 years (neonates excluded). RSV seasonality in Zaria runs from March to October.

Sudan
Gaafar Ibnauf Specialized Hospital, Khartoum, Sudan
Gaafar Ibnauf Specialized Hospital is a children’s hospital located in Khartoum, Sudan. It is the largest children’s hospital in Sudan and incorporates many of the pediatric subspecialties including respiratory medicine, neurology, gastroenterology, endocrinology, cardiology, nephrology, infectious diseases, pediatric intensive care, and neonatal intensive care. It was one of the first dedicated children’s hospitals in Africa. Gaafar Ibnauf Hospital provides medical care for children from all over Sudan. Moreover, this institution provides training for medical interns and pediatric residents.


Tanzania
Muhimbili National Hospital, Dar es Salaam, Tanzania
Muhimbili National Hospital is a national referral hospital located in Dar es Salaam, receiving patients from all regions of Tanzania. The PICU consists of 13 beds of which 11 beds have access to mechanical ventilation. Each month, approximately 30 patients are admitted to the PICU, of which the majority is <2 years old and an estimated 75% is admitted for respiratory problems. Most children with respiratory problems are admitted between December and May.
